Gamma Knife Treatment: A High-Efficacy, Non-Invasive Surgical Approach for Brain Disorders
Gamma Knife treatment is a high-efficacy, next-generation therapeutic method that allows neurosurgeons to perform surgery without making any incisions. Initially developed for brain tumors and vascular malformations, it is now used to treat a variety of brain disorders.
What is Gamma Knife?
Despite its name, Gamma Knife is not an actual knife. The system uses gamma rays emitted from 192 radioactive cobalt sources arranged around the patient’s head. These rays have energy levels that do not typically cause damage to surrounding brain tissue. The treatment is based on delivering a high dose of energy in a single session by focusing the gamma ray beams on the target tissue. The key advantage of Gamma Knife is that it delivers maximum energy to the target area while avoiding harm to healthy brain and surrounding tissues. The method is particularly successful for small tumors detected early or deep-seated brain tumors.
Conditions Treated with Gamma Knife
Gamma Knife is most commonly used to treat the following conditions:
-
Benign Brain Tumors:
- Meningiomas
- Acoustic neuromas
- Vestibular schwannomas
- Pituitary adenomas
- Corner tumors
-
Malignant Brain Tumors:
- Brain metastases
- Glial tumors
-
Vascular Brain Disorders:
- Arteriovenous malformations (AVM)
- Cavernomas
-
Functional Brain Disorders:
- Trigeminal neuralgia
- Parkinsonism
- Epilepsy
-
Neuropsychiatric Disorders:
- Obsessive-Compulsive Disorder (OCD)
-
Post-Surgical Tumor Recurrence:
- Residual or recurrent tumors after open brain surgery.
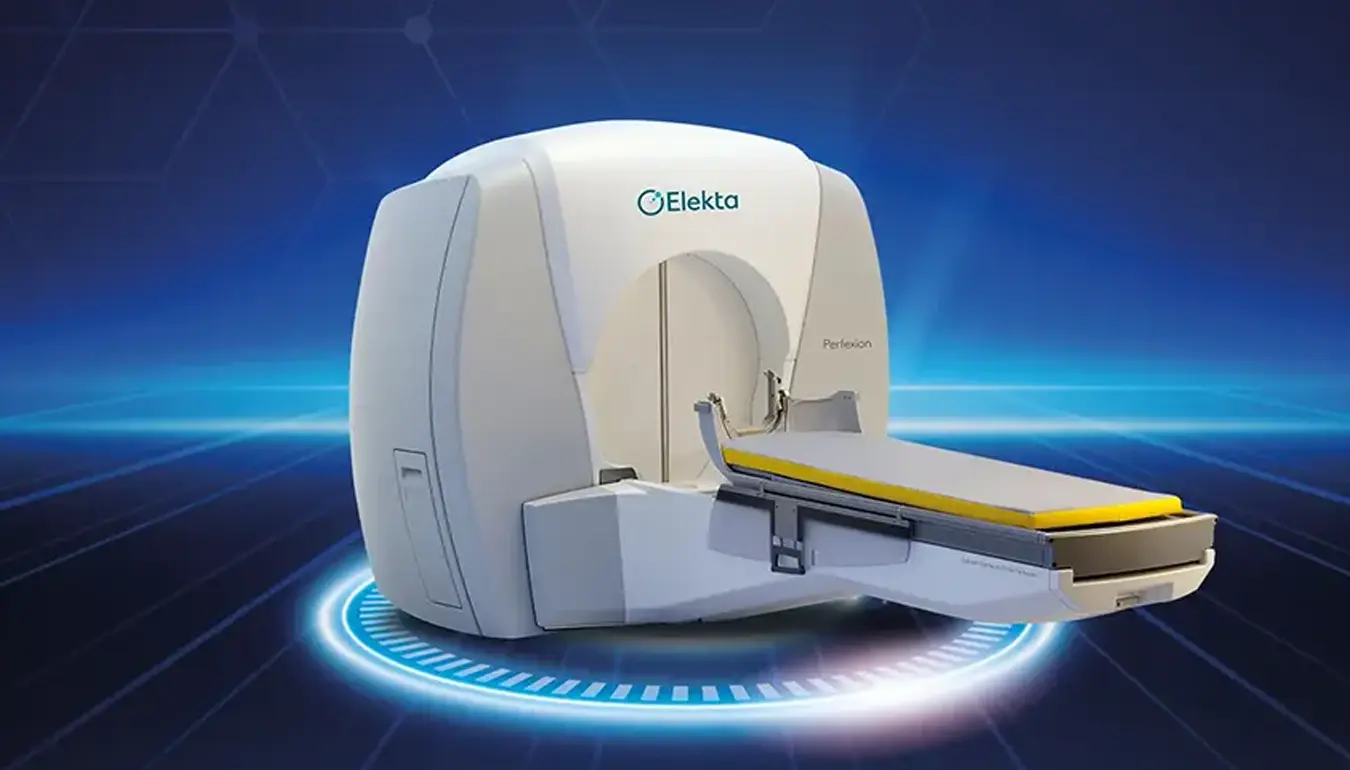
Gamma Knife Treatment Team at Koru Hospital
At Koru Hospital, the Gamma Knife treatment team is led by Assoc. Prof. Dr. Güner Menekşe, with Dr. Yunus Kaçar (Neurosurgeon) and Dr. Haluk Metin Aşıkoğlu (Radiation Oncology Specialist) on board. Our facility uses the Leksell Gamma Knife® Perfexion™ device.
How is Gamma Knife Treatment Applied?
-
Decision-Making and Preparation Patients who are candidates for Gamma Knife treatment are first evaluated in the Gamma Knife Council. Once a decision is made, a pre-procedure anesthesia evaluation is performed. The day before the treatment, a special contrast-enhanced Brain MRI scan is performed for treatment planning.
-
Stereotactic Frame Placement On the treatment day, the patient is brought to the Gamma Knife unit. A stereotactic frame is attached to the patient’s head using four pins after local anesthesia. This frame ensures that the treatment is applied with millimetric precision. The patient does not feel pain during this procedure.
-
Neuroradiological Imaging After the frame is placed, the patient is taken to the imaging center where appropriate diagnostic imaging is performed. For tumor cases, MRI or CT scans are used, while for vascular pathologies like AVMs, angiography with the stereotactic frame is performed.
-
Treatment Dose Planning Treatment planning is performed by the neurosurgeon using a specialized software (Leksell GammaPlan). The target tissue is precisely identified, and the radiation dose is calculated. The surrounding healthy tissue is protected. Thanks to the modern Leksell Gamma Knife® Perfexion™ device and the stereotactic frame, the treatment is applied with minimal deviation from the target area.
-
Applying the Treatment Once the treatment plan is finalized, the patient is positioned on a treatment table with the frame in place. During the procedure, the patient’s vital signs are monitored. The procedure is closely observed via audio and video surveillance for patient safety and comfort. Depending on the characteristics of the lesion, the treatment duration can vary between 15 minutes and 2 hours.
-
Finishing the Treatment After the treatment is completed, the patient is carefully removed from the platform. The stereotactic frame is removed, and a bandage is applied. The patient is observed briefly and can usually be discharged the same day without any complications. There are no travel restrictions after the treatment, and patients can resume normal activities immediately.
Key Differences of Gamma Knife Treatment
-
Non-invasive Surgical Technique: Gamma Knife is a non-invasive surgical treatment that does not require opening the skull. The procedure is pain-free, bloodless, and provides successful results without the need for traditional surgery.
-
Quick Return to Daily Life: Patients can often return to their normal social and work activities the very next day, without any loss of productivity or income.
-
Short Hospital Stay: Gamma Knife treatment does not require a lengthy hospital stay. Patients can be discharged the same day after a brief observation period, with no need for intensive care.
-
No General Anesthesia: Unlike conventional surgery, Gamma Knife does not require general anesthesia, making it suitable for elderly patients (over 65) or those with systemic or chronic diseases, and for those who may not tolerate open surgery.
-
Minimal Risk: The risk of permanent disability or death due to Gamma Knife treatment is very low.
-
Single Session Treatment: Unlike traditional brain radiotherapy, Gamma Knife treatment is completed in a single session, making it a faster option.
-
No Hair Loss: Unlike conventional radiotherapy, Gamma Knife treatment does not cause hair loss, and there is no need for hair shaving.
-
Precision in Radiation Delivery: Gamma Knife produces a sharper beam compared to other radiation therapies like CyberKnife or TrueBeam. It minimizes radiation exposure to healthy brain tissue, reducing the risk of neurological deficits.
-
Effective for Recurrent or Incomplete Tumor Removal: In cases where a tumor was not completely removed during open surgery, or if the tumor recurs, Gamma Knife offers a non-invasive solution without the need for further surgery.
-
Accompaniment for Patients: Family members or caregivers can stay in a designated rest area and accompany the patient during the procedure.
Why Choose Gamma Knife?
Gamma Knife is a highly effective treatment method for brain lesions, including tumors and vascular abnormalities, offering precision and minimal side effects. It allows patients to undergo treatment without the need for invasive surgery, enabling them to return to their normal activities much faster than traditional surgical approaches.